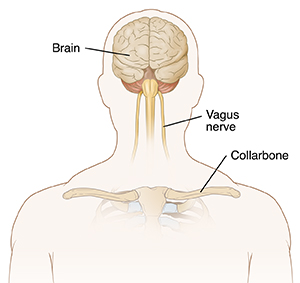
Having Vagus Nerve Stimulator Placement
A vagus nerve stimulator (VNS) is an electric device that can help prevent seizures. It can also treat depression, obesity, as well as other conditions. It has 2 parts: a pulse generator and leads. The pulse generator is the size and shape of a stopwatch, it is made of a battery and a computer chip. It's placed under your skin, usually below the collarbone. The leads run from the generator to a vagus nerve, deep in your neck. The VNS is put in your body during a surgery.
What to tell your healthcare provider
Before your surgery, tell your healthcare provider:
-
What medicines you take. This includes over-the-counter medicines, such as ibuprofen. It also includes vitamins, herbs, and other supplements. You may need to stop taking some medicines before the procedure, such as blood thinners and aspirin.
-
If you smoke. You may need to stop before your surgery. Smoking can delay healing. Talk with your healthcare provider if you need help to stop smoking.
-
If you’ve had recent changes in your health. This includes an infection or fever.
-
If you are sensitive or allergic to anything. This includes medicines, latex, tape, and anesthetic medicines.
-
If you are pregnant. Tell your healthcare provider if you think you may be pregnant.
-
About your entire health history. Some health problems may not be good with VNS placement. These include a history of fainting and certain lung diseases.
Getting ready for your surgery
Make sure to:
-
Ask a family member or friend to take you home from the hospital
-
Make plans for some help at home while you recover
-
Follow all other directions from your healthcare provider
-
Read the consent form and ask questions if something is not clear
-
Not eat or drink after midnight before your surgery
Tests before your surgery
Before your surgery, you may need tests such as:
-
Blood tests, to check your general health
-
Chest X-ray
-
Electrocardiogram (ECG), to check the heart rhythm
-
Video electroencephalogram to see where seizures occur in your brain
On the day of your surgery
Your procedure will be done by a brain surgeon (neurosurgeon), a vascular surgeon, or a healthcare provider who treats ear, nose, and throat conditions (otolaryngologist). They will work with a team of specialized nurses. The surgery can be done in several ways. Ask your healthcare provider about the details of your surgery. The whole procedure may take a couple of hours. In general, you can expect the following:
-
You will have general anesthesia, a medicine that allows you to sleep through the surgery. You won’t feel any pain during the surgery.
-
A healthcare provider will watch your heart rate, blood pressure, and other vital signs during the surgery.
-
You may be given antibiotics during and after the surgery. This is to help prevent infection.
-
The surgical team will clean the left side of your neck and chest. The surgeon will make a small cut (incision) in each spot.
-
The surgeon will move your neck tissues and muscles out of the way so they can find your left vagus nerve.
-
The surgeon will create a small pocket between the muscles and skin of your chest. They will then create a tunnel. The leads will be passed through the tunnel. They will wrap the ends of the leads around your left vagus nerve.
-
Once the leads are connected to the pulse generator, the surgical team will test the VNS.
-
The surgeon will put the pulse generator in the pocket in your chest.
-
The surgeon will close the skin with stitches (sutures). A bandage will be put on the area.
After your surgery
After the surgery, you will spend several hours in a recovery room. You may be sleepy and confused when you wake up. Your healthcare team will watch your heart rate, breathing, and other vital signs. You’ll be given pain medicine if you need it.
You can resume a normal diet as soon as you are able. You will likely go home that day once you are feeling better. The surgeon may give you a prescription for pain medicine.
Recovering at home
Follow all the directions your healthcare provider gives you for medicines, exercise, diet, and wound care. Keep an eye on your incisions as they heal. You may notice a small amount of fluid leaking from them. This is normal during the first few days.
Follow-up care
Make sure to keep all your follow-up appointments. This is so your healthcare provider can check your progress. About 2 weeks after your surgery, your healthcare provider will turn on your VNS. Once it’s turned on, your healthcare provider can change the settings at follow-up visits if needed.
Managing your VNS
Talk with your healthcare provider about how to best use your VNS. You will need to:
-
Use a magnet, if directed. If you have auras before your seizures, you may be able to use a magnet to activate your VNS. This may alter or prevent a seizure from happening. Auras are symptoms that occur before a seizure.
-
Don't do certain things. Talk with your healthcare provider about what you can't do once your VNS is in place. You may not be able to have some types of MRI tests. You may not be able to have heat treatments that use shortwaves or microwaves.
-
Take your medicines as directed. You will continue to need medicines to control your seizures. But if the VNS works well for you, your healthcare provider may lower your dose. Or you may be able to stop taking certain medicines.
-
Have the battery replaced when needed. Over time, the battery’s power will drain. Eventually you will need to have the battery of your VNS replaced. This can often be done as an outpatient procedure using the existing leads. It's important to replace the battery before it loses power.
You may notice that your seizure control continues to improve over the next several years. You may also notice improvements in your mood. You may feel more alert and less sleepy during the day.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following occur: