Knee Arthroscopy for a Ligament Tear
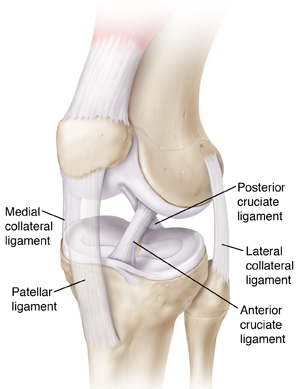
Ligaments are strong bands of tissue that help support the knee. A ligament tear can cause pain or swelling. It can also cause the knee to feel unstable. Knee arthroscopy is a procedure that can diagnose and treat a ligament tear. It's done with a device called an arthroscope (scope). The scope is a thin tube containing a light and camera. It allows the orthopedic surgeon to see and work inside the knee joint. This sheet tells you more about the procedure and what to expect.
Preparing for surgery
Prepare as you have been told. Tell your surgeon about all medicines you take. This includes over-the-counter medicines. It also includes herbs and other supplements. You may need to stop taking some or all of them before surgery. Also, follow any directions you’re given for not eating or drinking before surgery.
The day of surgery
The surgery takes about 1 to 2 hours. You will likely go home the same day.
Before the surgery begins:
-
Medical staff will put an IV line into a vein in your arm or hand. This line supplies fluids and medicines.
-
You will be given medicine to keep you free of pain during the surgery. This is called anesthesia. Depending on what type of anesthesia is used, you may be awake, drowsy, or asleep during the surgery. You may also be given medicine in the area of your leg that will be worked on.
-
Staff will mark the knee to be worked on.
During the surgery:
-
The surgeon makes 2 or 3 small cuts (portals) in the knee. In some cases, you may need a slightly larger incision.
-
The surgeon will put a scope through one of the portals. It sends pictures from inside the knee to a video screen. Sterile fluid is sent through the scope to expand the knee joint. The fluid makes it easier to see the knee joint. The healthcare provider looks closely at the tear and determines how best to treat it.
-
The surgeon puts surgical tools through the other portals.
-
The scope and tools are used to reconstruct a torn ligament. Damaged tissue is replaced with a piece of healthy tissue (a graft). The graft tissue may come from your own body or from a tissue donor.
-
When the procedure is done, the surgeon drains sterile fluid from the knee. The scope and other tools are removed.
-
Incisions are closed with stitches (sutures). The knee is then bandaged.
After the surgery
You’ll be taken to a recovery room. Medicines and cold packs are often used to manage pain and swelling. Your leg is also raised to reduce swelling. You may be given a special brace to wear. This brace helps support the knee while it heals. When it’s time to go home, have an adult friend or family member drive you.
Recovering at home
Once home, follow any instructions you are given. These include:
-
Take pain medicine and any other medicine as directed.
-
Care for your incisions as instructed. This includes keeping the incisions dry when bathing or showering.
-
Elevate your leg to reduce pain and swelling. This means keeping your knee at a level higher than your heart.
-
Apply an ice pack wrapped in a thin towel to your knee to reduce swelling a few times a day. Do this for 20 minutes at a time. Or use a continuous icing system if recommended by your healthcare provider. Icing helps reduce swelling.
-
Expect some numbness in the leg for 24 to 28 hours after surgery, especially if local numbing medicine was used.
-
Do exercises to help with healing as instructed. You may be told to walk a few times daily.
-
Use any aids, such as a brace, splint, or crutches, as instructed.
-
Limit sports or activities as directed.
-
Don't drive until your healthcare provider says it’s OK.
-
Do physical therapy (PT) for your knee as prescribed. PT is a program of guided exercise that can help you regain movement and strength in your knee.
When to call your healthcare provider
Call the healthcare provider if you have any of the following:
-
Fever of 100.4° F ( 38° C) or higher, or as directed by your healthcare provider
-
Chills
-
Pain that isn’t helped by medicine and rest
-
Increased swelling not helped by elevation and cold packs
-
Signs of infection at any incision site such as increased redness or swelling, warmth, worsening pain, or foul-smelling drainage
-
Bleeding through the bandages
-
Worsening numbness in the leg
-
Severe nausea
-
Any other signs or symptoms indicated by your healthcare provider
Call 911
Call 911 if you have any of the following:
Follow-up care
Keep all follow-up appointments with your healthcare provider. Stitches will likely need to be removed about 7 to 14 days after surgery. If physical therapy is prescribed, keep all appointments with your physical therapist. They can help you set goals for recovery and a plan to work toward them. Be patient with your progress. Your length of recovery will depend on the type of damage that was present in your knee and the treatment necessary.
Risks and possible complications
-
Infection
-
Bleeding
-
Blood clots
-
Stiffness or ongoing pain in the knee
-
Damage to the blood vessels, nerves, or skin around the knee
-
Damage to the cartilage, meniscus, or ligaments in the knee
-
Increased pressure in the leg due to swelling
-
Need for further surgery
-
Risks of anesthesia. The anesthesiologist will discuss these with you.