Meningitis
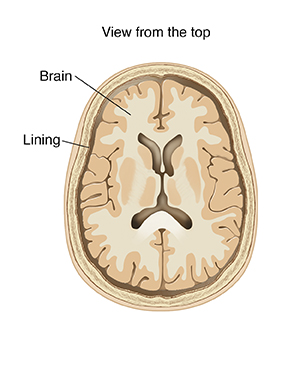
Meningitis is inflammation of the lining around the brain and spinal cord (meninges). It’s most often caused by germs that infect the fluid and lining. Types of meningitis include:
-
Bacterial meningitis. This is caused by bacteria. It is a serious illness that can lead to lasting problems. These include brain damage, hearing loss, and paralysis. When not treated quickly, it can cause death, sometimes within days.
-
Viral meningitis. This is caused by a virus. It is less serious than bacterial meningitis. Most people get better with supportive treatment.
-
Fungal meningitis. This is caused by breathing in fungal spores. It is often very serious. This often occurs only in people with immune system disorders such as cancer or AIDS.
-
Aseptic meningitis. This occurs when there is inflammation of the meninges without bacteria being found. This is often caused by viral or fungal infections. But it can occur as a reaction to certain medicines.
What are the risk factors for meningitis?
Anyone can get this condition. These people are at greatest risk:
-
Children younger than 5
-
Older adults
-
People who've had their spleen removed
-
People who are more likely to come in contact with meningitis germs (such as children in daycare, students in college dorms, and soldiers in military housing)
How does meningitis spread?
-
Droplets. Meningitis germs spread through the air in droplets when an infected person coughs, sneezes, laughs, or talks. You can breathe in the germs. Or, your hands can transfer the germs to your eyes, nose, or mouth.
-
Person-to-person. You can come in contact with the germs if you share food, a drinking glass, eating utensils, or a toothbrush with an infected person. Meningitis germs can also be spread through kissing.
-
Direct spread. The germs that cause meningitis can spread to the brain and spinal cord from an infection in another part of the body, such as the sinuses or ears.
-
Fecal-oral. People infected with viral meningitis have the virus in their stool. If they don’t wash their hands well after using the bathroom, they can spread the germs to objects, such as phones and doorknobs. If you touch the same objects, you can pick up the germs and then transfer them to your mouth.
What are the symptoms of meningitis?
Viral and bacterial meningitis share many of the same symptoms. Symptoms start suddenly in both. You won’t know which type of meningitis you have, so act quickly. Call your healthcare provider right away or get immediate medical care if you have a severe headache with any of the following:
-
Stiff neck
-
Fever
-
Confusion
-
Sleepiness
-
Seizures
-
Sensitivity to light
-
Nausea and vomiting
-
Paralysis or weakness
Note: Small children, older adults, and occasionally other people may not have headaches as an early symptom of meningitis. Unexplained confusion even without headache can occasionally be due to meningitis.
How is meningitis diagnosed?
The following are tests used to diagnose meningitis:
-
Lumbar puncture (spinal tap). This is the best way to diagnose meningitis. The healthcare provider first injects a numbing medicine to ease pain. Then, a needle is inserted into the back to take a small sample of the fluid that surrounds the brain and spine.
-
Imaging tests. MRI or CT scans of the brain may be done to look for swelling and inflammation. Other CT scans and X-rays may be done to look for a source of the infection.
How is viral meningitis treated?
There are no medicines to treat most types of viral meningitis. It often resolves on its own in about a week. After you have had a medical evaluation, the following may help with your symptoms:
-
Rest in bed.
-
Drink plenty of fluids, such as water, juice, and warm soup, to prevent dehydration. A good rule is to drink enough so that you pee your normal amount.
-
Ask your healthcare provider about over-the-counter medicines for headache and fever.
-
Avoid bright lights, which may bother your eyes.
-
Call your provider if symptoms get worse or there are signs of dehydration. These include a dry mouth, intense thirst, and little or no peeing.
How is bacterial or fungal meningitis treated?
Urgent or emergency hospital care is needed for bacterial or fungal meningitis. In the hospital, fluids and antibiotics are given through an IV (intravenous) line. Medicine to reduce inflammation may also be given. When symptoms are severe, a tube to aid breathing may be needed. People with fungal or tuberculous meningitis may need medicine for a prolonged time.
Vaccines for bacterial meningitis
There are several different vaccines for different types of bacterial meningitis.
The Haemophilus influenzae type b (Hib) vaccine prevents meningitis caused by a type of bacteria called Haemophilus influenzae type b. It's recommended for all children younger than 5 years old. It's usually given to infants starting at 2 months of age as a series.
Pneumococcal bacteria can also cause meningitis. The pneumococcal conjugate vaccine, PCV13, protects against the 13 types that cause the most severe pneumococcal infections. PCV13 is given to infants and toddlers. But it may be given to older children as well. A dose is also recommended to older children who are at high risk. Another vaccine, PPSV23, is given to older children with certain chronic medical conditions.
Another type of meningitis is meningococcal meningitis. Vaccination is recommended beginning in children at age 11 through the age of 16. Catch-up vaccines may be given at age 13 to 15 years or 16 to 18 years. College freshmen living in dorms are one group at high risk. Vaccination is also recommended for those at high risk beginning at age 2 months through 10 years. High-risk infants and children include those:
-
With specific medical conditions:
-
Complement component deficiencies (immune system condition with increased risk of serious infections)
-
Functional or anatomic asplenia (meaning that the spleen does not work effectively or has been removed), including those with sickle cell disease
-
Who live in an area where there is a meningococcal disease outbreak
-
Who travel to areas where meningococcal diseases are common or where there is an outbreak
To help prevent meningitis
Here are some tips to follow:
-
Wash your hands often with soap and clean, running water. If you can’t wash your hands, use an alcohol-based hand gel containing at least 60% alcohol.
-
Don't share personal items, such as food, drinking glasses, eating utensils, or towels.
-
If you've had close contact with someone who has meningitis, ask your healthcare provider if you should take antibiotics to prevent infection.