When Your Child Has Ewing Sarcoma
Your child has been diagnosed with Ewing sarcoma. You likely feel shocked and scared. But you're not alone. Your child’s healthcare team will help you as you make important decisions about your child’s health and cancer treatment.
What is Ewing sarcoma?
Ewing sarcoma is a type of cancer that starts in bone or soft tissue, such as muscle. It can start anywhere in the skeleton. It's most often found in the chest wall (ribs or shoulder blades), hip bones (pelvis), and legs. The cancer cells grow fast. They can spread (metastasize) to another part of the body, like the lungs or other bones.
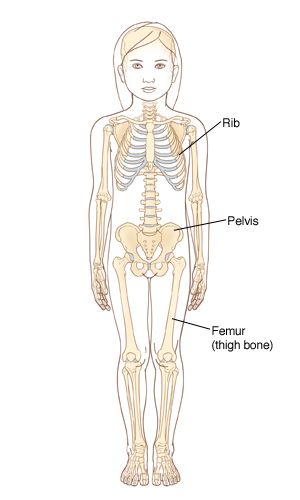 |
| Ewing sarcoma usually forms in bone. Some common sites include the ribs, pelvis, and thigh bones. |
Who gets Ewing sarcoma?
Children at any age can get Ewing sarcoma, but it's most often found in teenagers. It's rare in adults.
What causes Ewing sarcoma?
Ewing sarcoma happens because cells change and grow out of control. These cells then form a tumor. What causes the change (mutation) in the cells is not known.
What are the symptoms of Ewing sarcoma?
Some common symptoms of Ewing sarcoma include pain or a lump or swelling in the arms, legs, chest, pelvis, or back. Sometimes a bone breaks (fractures) for no known reason.
How is Ewing sarcoma diagnosed?
Your child’s healthcare provider will examine your child. You'll be asked about your child’s health history. One or more of these tests may be done:
-
Imaging tests to take detailed pictures of the inside of your child's body. These may include an X-ray, MRI, CT scan, PET scan, or bone scan.
-
A biopsy to take out tiny pieces (samples) of the tumor to test them for cancer.
-
A bone marrow aspiration and biopsy to take out small pieces of bone marrow from the back of the hipbone and test them for cancer.
-
Blood tests to measure certain substances and blood cell counts.
Is it localized or metastatic?
To decide on the best treatment plan and likely outcome (prognosis) for your child, the healthcare team looks at many things. These include how big the tumor is, where it is, and if it has spread.
Both treatment and prognosis depend on whether the tumor affects only one part of the body (localized Ewing sarcoma) or has spread to more than 1 part of the body (metastatic Ewing sarcoma).
Your child’s healthcare provider will talk with you about how far your child's cancer is thought to have spread and what it means for your child.
How is Ewing sarcoma treated?
The goal of treatment is to take out or kill cancer cells. The kind of treatment your child gets depends on the size of the tumor, where it is, and whether the cancer is localized or metastatic. Your child may need 1 or more of these treatments:
-
Chemotherapy (chemo) uses strong medicines to kill cancer cells. More than 1 chemo medicine may be used. They're given through a tube (IV or intravenous line) that’s usually put into a vein in the arm or chest. Sometimes they can be given by mouth or as a shot (injection).
-
Surgery is done to take out all or part of the tumor.
-
Radiation therapy kills cancer cells and shrinks tumors using high-energy X-rays. Radiation may be used before or after other treatments.
-
High-dose chemotherapy and stem cell transplant may be an option if the cancer has certain features or if other treatments don't work.
Supportive therapy
The goal of supportive therapy is to help your child feel better. It can be used to do things like help prevent infection, ease pain, and help keep blood counts within a healthy range. For instance, during your child’s treatment, antibiotics may be needed. These are medicines that help prevent and fight infection. Your child may need a blood transfusion or medicines to restore blood cells destroyed by treatment. Anti-nausea medicines, pain medicines, and other medicines may also be given. These help ease side effects caused by the cancer and cancer treatment.
What are the long-term concerns?
Your child may need physical therapy. This is to help get the body working after treatment. Also, chemotherapy and radiation may cause some problems. This can include damage to certain organs, changes in growth, fertility problems, and a higher-than-normal risk for cancer later in life. All this means that your child’s health will need medical follow-up for life. This may include clinic visits, blood tests, imaging of the heart, and other scans and imaging tests.
Coping
Being told your child has cancer is scary and confusing. It’s important to remember that you're not alone. Your child’s healthcare team will work with you, your family, and your child during your child’s illness and care. You may also want to learn more about this cancer and get support for yourself and the rest of your family. Doing so can help you all cope with the changes cancer brings. Learning about and talking with others who also have a child with cancer may help you and your family cope, too. Some helpful resources include: